For Concerned Others
If someone you know is experiencing depression, do not criticize him or her or give advice. Instead, connect the individual to someone who can help. There are psychologists and social workers on staff for most area school districts. An individual’s school counselor often can be a good starting point for encouraging a student to receive assistance.
Notice and pay attention to any extreme changes, which can occur over a long period of time. Five signs that someone may need help include a personality change, agitation, being withdrawn, exhibiting poor self-care and appearing hopeless. Other indications of possible mental health issues include extreme aggressiveness, low toleration for frustration, the inability to store or retrieve information, forgotten materials or assignments, and frequent absences or trips to the school nurse.

Statements or actions that mean someone could need assistance include remarking “I don’t see the point in life,” talking about self-injuring, engaging in reckless or dangerous behaviors, being increasingly absent from school and/or having significant substance abuse issues. Remember the “ACT” acronym: Acknowledge, Care, Tell. Acknowledge/validate the person’s feelings and take any comment about death or self harm seriously. Care by assuring the individual that you will help him or her remain safe and obtain help. Let the person know that he or she is important to you and that his or her life has value. If you are a youth, Tell an adult the whole truth (in case the individual is not comfortable disclosing everything) immediately. You can text NEEDHELP to 85511, contact Crisis Link at (703) 527-4077 or call 911 in case of emergency. Never promise to keep a secret if you believe a person might hurt themselves. Share concerns about social media posts with a trusted adult.
Intervention language is intended to connect youth, who are exhibiting concerning behavior, to the right type of help. You can begin by saying, “Is everything okay, I have noticed that you have been…”. Let the individual know you care, by following up with, “I’m concerned. This is not typical for you. You deserve to feel better.” Continue with, “What can I do to help? Let’s come up with a solution together.” If there is indeed reason for concern, develop an action plan with the youth and make sure he or she becomes connected with school or community resources as appropriate.

If you are a parent who is concerned about your child, a visit to his or her pediatrician can be a helpful first step. There can be primary medical reasons for depression. For instance, Lyme disease can mimic psychiatric disorders and increase the severity of prior underlying symptoms. There also is growing evidence that anemia can be a cause of depression in children rather than simply a chance association. Depression is common in individuals with Attention-Deficit/Hyperactivity Disorder (ADHD). CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) estimates that approximately 14 percent of children with ADHD have depression as compared to only 1 percent of those without ADHD. The use of marijuana and other illicit drugs can cause or worsen depression in adolescents. (According to the Office of National Drug Control Policy, using marijuana weekly or more frequently doubles a teen’s risk for depression and anxiety. Similarly, depressed youth are more than twice as likely as their peers to abuse or become dependent upon marijuana.)
Cultural competence is a health care provider’s ability to recognize and understand the role that his or her culture along with the patient’s has in treatment. An individual’s beliefs, values and language can affect how mental health conditions are viewed and symptoms are described, whether and what type of help is sought, how a patient communicates with health care providers and which treatments might be successful. Diverse communities often face barriers to care, which include higher levels of stigma, misinformation about mental health, and language. To combat this, contact providers or agencies from your cultural background or look for ones that have worked with people who have a similar cultural background. Search online or ask for referrals from cultural organizations in your community. You also can contact your health insurance plan about providers, who fit your cultural background and/or are bilingual.
A study in the May/June 2017 issue of Child Development, which focused on teenage girls, found that nighttime usage of a cell phone can increase depression and anxiety in adolescents due to disrupted sleep. Possible solutions to the problem include placing a power strip in parents’ bedrooms to have all of the technology (including cell phones) charged there overnight. Experts recommend that teens who use their phones as alarms replace them with clocks in order to maintain an electronic curfew. Adolescents need 8 to 10 hours of sleep each night and cell phones affect that in two ways, with their screens’ bright light disrupting natural circadian rhythms and through the sending and receiving of text messages, which continues well past bedtime for most teens.
Pharmacogenetic testing, which is conducted with cheek swabs or blood or saliva samples, is now available. The results allow healthcare providers to better understand how patients will process and metabolize certain prescription medications, including numerous antidepressants, and permit better and more informed medication therapy decisions for depression.

Supplements, such as L-methylfolate, a form of B vitamin, have been shown to help individuals who have not had a good response to treatment with antidepressant medication and can be combined with antidepressants under the care and advice of a doctor, who will consider a youth’s medical history and conduct a physical examination before prescribing L-methylfolate.
Transcranial magnetic stimulation (TMS), a noninvasive procedure using magnetic fields to stimulate nerve cells in the brain that is used in a milder form in children and adolescents, can sometimes improve symptoms of depression when other treatments have not been effective. (In adults, TMS typically is administered five times a week for a total of 30 sessions over a four to six week period.)

Recognize the signs of youth stress: headaches, stomachaches, dizziness, chest pain and changes in appetite and sleeping patterns. A Mental Health Screening Tool for youth, the Pediatric Symptom Checklist, can be found on Mental Health America’s (MHA) website. http://www.mentalhealthamerica.net/mental-health-screen/youth MHA, which was founded in 1909 is a community-based nonprofit that addresses the needs of those living with mental illness and promotes Americans’ overall mental health. There also is a Parent Test (for child) http://www.mentalhealthamerica.net/mental-health-screen/parents and a Depression Screening Tool in Spanish http://www.mentalhealthamerica.net/mental-health-spanish-screen/spanish-depression.
While the Diagnostic and Statistical Manual, Fifth Edition lists symptoms of adult depression as: (1) being in a depressed mood for most of the day, nearly every day; (2) loss of interest or pleasure in all, or almost all, activities; (3) significant weight loss or gain; (4) insomnia or excessive daytime sleepiness; and/or (5) series of unintentional or purposeless motions, such as pacing or wringing one’s hands, clinicians more often observe irritability or hyperactivity as the major symptoms of depression in youth.

Ensure that the individual is not suicidal. If someone has a plan for committing suicide, he or she is at high risk for actually taking action. Any “half-hearted” suicide attempt should be taken seriously. The first step to combating suicide is awareness. The “Ask Suicide-Screening Questions” Suicide Risk Screening Tool can be found on the National Institute of Mental Health’s website (https://www.nimh.nih.gov/news/science-news/ask-suicide-screening-questions-asq.shtml).
Talking openly and honestly about emotional distress and suicide will not make someone more suicidal. If you are concerned about an individual, ask him or her about your worries. Do not judge the person or his or her thoughts, instead listen in a caring and kind way. Offer to stay with the individual, to accompany him or her to get help and/or to assist him or her in contacting a crisis line.

Trauma has been identified as a central issue for individuals with mental health problems. It has been estimated that 82 percent of young people in inpatient and residential treatment programs and 93 percent of psychiatrically hospitalized adolescents have histories of trauma. After a trauma, assure youths that they are safe. Explain that they are not responsible for what happened. (Children often blame themselves for events which are completely out of their control.) Reassure them by saying, “It is not your fault.”; “You are a good person that had a bad thing happen.”; “People care about you.” and “You are strong.” While some individuals will recover quickly, others may not. Be patient and reassure them that their feelings are nothing to feel guilty about. Mental health professionals trained in trauma treatment can help youth and their families cope and heal.
Families can have a positive influence on their youths’ recovery. Research has demonstrated that family psychoeducation and support can help reduce relapse rates and improve recovery outcomes and overall family well-being. Love, understanding, and regular communication are some of the most important things a parent can provide to help his or her child cope with depression. A supportive family environment can include simple things like having your child eat small snacks rather than large meals if he or she lacks an appetite and being hopeful about his or her recovery. If your child has trouble sleeping, establish a consistent bedtime, keep his or her bedroom dark and quiet, and discourage him or her from exercising after 5:00 p.m. Finally, positive thinking is very important in treating depression, so remind your child that improvement occurs gradually and takes time.
Many of the above tips were gathered from Fairfax County Public Schools’ “Student Wellness: Tips and Strategies,” Kognito’s “At-risk: Friends in College” training and Fairfax County’s At-Risk Youth Suicide Prevention Training.
For Youth Suffering from Depression
If you are a homeless or unaccompanied teenager without proper care from a parent or guardian, you may contact the Fairfax County Public Schools Homeless Liaison at (571) 423-4332 for assistance.
Speak to the adults in your life about how you are feeling and write down the name of one you can go to if you need help. Ask for assistance and support when you need it.
The Fairfax County Youth Survey showed that having just “Three to Succeed” Assets promotes youth’s mental and physical health. Besides “Having Community Adults to Talk to”, the other Assets include: (1) Having High Personal Integrity, (2) Performing Community Service, (3) Participating in Extracurricular Activities, (4) Having Teachers Recognize Good Work and (5) Having Parents Available for Help.

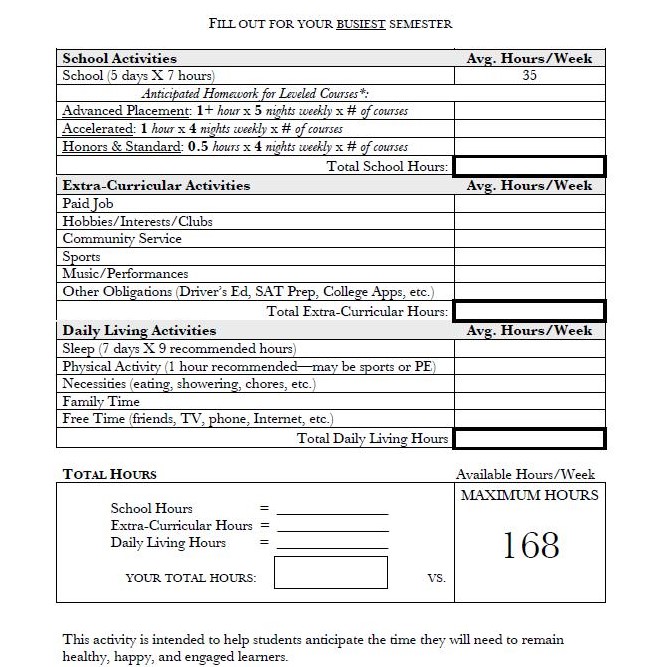
Limit Advanced Placement classes and extracurricular activities to the ones you enjoy. Have reasonable expectations and boundaries. Fill out this Time Management Activity to avoid over-scheduling.
Spend time with your favorite people. Unplug, slow down and reflect on the important things in life. Make time for the things you enjoy and that bring you happiness. Relax by going on a hike, meditating or taking a bubble bath.
Get 8 to 10 hours of sleep each night and exercise three or more times each week. Avoid drugs and alcohol.

Continuity of care is very important for a successful transition from high school to college, especially during Freshman year. Begin planning before you graduate, especially if you are taking psychotropic medication or have been psychiatrically hospitalized. Do not allow the pressure of having to build a relationship with a new therapist or doctor deter you from continuing treatment in college, even if you are very happy with your current one. Remember the importance of self care in college, including sleeping, eating well and getting enough exercise. Find helpful information for “Treatment in College” at https://www.erikaslighthouse.org/young-adults.
Co–rumination or extensively discussing problems and focusing on negative feelings with your peers can actually worsen depression and raise anxiety, especially in girls. Healthy alternatives include, distracting yourself with meditation or prayer; taking small steps to begin solving problems; reconsidering negative thoughts about events and/or other people’s expectations; and letting go of unattainable goals.
Many of the above tips for youth were gathered from the “Race to Nowhere”.